Regular visits to the dentist might help keep joint pain at bay, too.

When Rice University computational biologist Vicky Yao found traces of bacteria associated with periodontal disease in samples collected from rheumatoid arthritis patients, she was not sure what to make of it.
Her finding helped spark a series of experiments that confirmed a connection between arthritis flare-ups and periodontitis. The study is published in Science Translational Medicine.
Tracing this connection between the two conditions could help develop therapies for rheumatoid arthritis, an autoimmune inflammatory disease that attacks the lining of the joints and can cause heart, lung and eye problems. The approach that led to the study could prove fruitful in other disease contexts, such as cancer.
“Data gathered in experiments from living organisms or cells or tissue grown in petri dishes is really important to confirm hypotheses, but, at the same time, this data perhaps holds more information than we are immediately able to derive from it,” Yao said.
Yao’s hunch was confirmed when she took a deeper look into data collected from rheumatoid arthritis patients by Dana Orange, an associate professor of clinical investigation and a rheumatologist, and Bob Darnell, a professor and attending physician at Rockefeller University and the Howard Hughes Medical Institute.
Yao was collaborating with Orange and others on a different project that tracked changes in gene expression during rheumatoid arthritis flare-ups.
“Orange, working with Darnell, collected data from arthritis patients at regular intervals while, at the same time, monitoring when the flares happened,” Yao said. “The idea was that perhaps looking at this data retroactively, some pattern would become visible giving clues as to what might cause the arthritis to flare up.
“While I was working on that project, I went to this talk that I thought was really cool because it pointed out that in the data that gets ignored or thrown out, you can actually find traces of microbes. You’re looking at a human sample but you get a snapshot of the microbes floating around. I was intrigued by this.”
When she looked into it, Yao found that the germs in the samples that changed consistently across patients prior to flares were largely ones associated with gum disease.
“I was curious about this tool that allowed you to detect microbes in human samples. It was sort of like, for free, you’re getting an extra perspective on the data,” Yao said. “At the time, I hadn’t worked much on microbial data at all. Since then, Dana leveraged all this expertise and got together with people studying these bacteria.
“One of the things that came up when we were discussing this was, how cool would it be if you could prescribe some kind of mouthwash to help prevent rheumatoid arthritis flares.”
Yao’s focus since joining Rice in 2019 has shifted to cancer research. The discovery of meaningful information in data that would usually be ignored or discarded inspired Yao to take a similar approach in looking at data from cancer patients.
“I got really interested in what else we can find mining for microbial signatures in human samples,” Yao said. “Now, we’re doing something similar in looking at cancer.
“The hope here is that if we find some interesting microbial or viral signatures that are associated with cancer, we can then identify productive experimental directions to pursue. For instance, if having a tumor creates this hotbed of specific microbes that we recognize, then we can maybe use that knowledge as a means to diagnose the cancer sooner or in a less invasive or costly way. Or, if you have microbes that have a very strong association with survival rates, that can help with prognosis. And if experiments confirm a causal link between a specific virus or bacteria and a type of cancer, then, of course, that could be useful for therapeutics.”
One of the better known examples of a pathogen associated with cancer is the human papillomavirus (HPV). Yao used this well-documented connection to verify her approach.
“When we did the same exercise looking at cervical cancer tumor samples, we consistently detected the virus,” she said. “It’s a nice proof-of-principle finding that shows that the presence of specific pathogens can be meaningful for certain types of cancer.
“I’m really interested in using computational approaches to bridge the gap between available experimental data and ways to interpret it. Computational analysis is a way to help interpret data and prioritize hypotheses for clinicians or experimental scientists to test.”
The National Institutes of Health (R01 AR063676, R01 AR078268, U19 AI110491, U01 AI101981, T32 HG003284, R01 GM071966, T32 AI007290-35, P30 AR079369), the National Science Foundation Graduate Research Fellowship, the Robertson Foundation, Rockefeller University (UL1 TR001866), the Bernard and Irene Schwartz Foundation, the Iris and Jungming Le Foundation, Rockefeller Clinical and Translational Science Award Program Pilot Award, the Rheumatology Research Foundation and the National Cancer Institute (F30 CA243480) supported the research.
-30-
- Peer-reviewed paper:
-
Oral mucosal breaks trigger anti-citrullinated bacterial and human protein antibody responses in rheumatoid arthritis | Science Translational Medicine | DOI: 10.1126/scitranslmed.abq8476
Authors: Camille Brewer, Tobias Lanz, Caryn Hale, Gregory Sepich-Poore, Cameron Martino, Austin Swafford, Thomas Carroll, Sarah Kongpachith, Lisa Blum, Serra Elliott, Nathalie Blachere, Salina Parveen, John Fak, Vicky Yao, Olga Troyanskaya, Mayu Frank, Michelle Bloom, Shaghayegh Jahanbani, Alejandro Gomez, Radhika Iyer, Nitya Ramadoss, Orr Sharpe, Sangeetha Chandrasekaran, Lindsay Kelmenson, Qian Wang, Heidi Wong, Holly Torres, Mark Wiensen, Dana Graves, Kevin Deane, Michael Holers, Rob Knight, Robert Darnell, William Robinson and Dana Orange
https://doi.org/10.1126/scitranslmed.abq8476 - Image downloads:
-
https://news-network.rice.edu/news/files/2023/03/vy-headshot.jpeg
CAPTION: Vicky Yao is an assistant professor of computer science at Rice University. (Photo by Ruth Dannenfelser/Rice University)
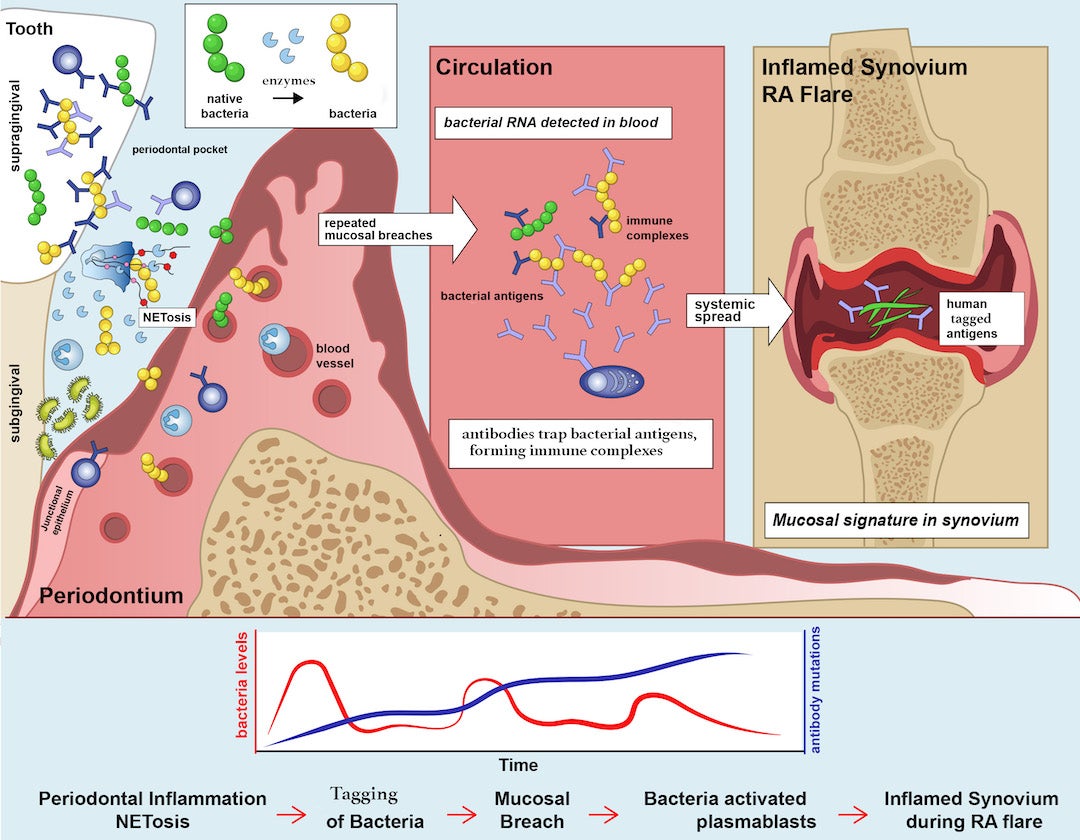
https://news-network.rice.edu/news/files/2023/03/fig8.jpgCAPTION: Proposed model for the role of periodontal inflammation in rheumatoid arthritis (RA). Periodontal inflammation is associated with a chemical change in supragingival bacteria caused by an enzyme released as part of an immune response mechanism known as NETosis. This chemical change ‘decorates’ bacterial antigens with a molecular tag. Periodontitis and inflammation can cause breaches of the mucous membrane lining inside the mouth, releasing the tagged bacterial antigens into the blood. As a result, antibodies that target these molecular tags are activated, and they bind or trap the tagged antigens, forming molecules known as immune complexes. Immune complexes and plasmablasts deposit in joint tissue, also known as synovium, and contribute to its inflammation. Repeated episodes of oral bacteremia cause a heightened autoimmune response, affecting join tissue. (Image courtesy of Dana Orange and Bill Robinson)
- Related stories:
-
Vicky Yao wins CAREER Award:
https://news.rice.edu/news/2022/vicky-yao-wins-career-award
Cells may tell if arthritis flare-ups are coming:https://news.rice.edu/news/2020/cells-may-tell-if-arthritis-flare-ups-are-coming
Study finds new link between Alzheimer’s suspects:
https://news.rice.edu/news/2020/study-finds-new-link-between-alzheimers-suspects - Links:
-
Yao lab: https://www.cs.rice.edu/~vy/
Rice Department of Computer Science: csweb.rice.eduGeorge R. Brown School of Engineering: engineering.rice.edu
- About Rice:
-
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation’s top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 4,552 undergraduates and 3,998 graduate students, Rice’s undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for lots of race/class interaction and No. 1 for quality of life by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger’s Personal Finance.