Acute myeloid leukemia (AML) remains one of the most aggressive and deadly forms of blood cancer, even as treatments have advanced in recent years. Standard approaches like high-dose chemotherapy and bone marrow transplants can extend life but often come at the cost of severe side effects — and many patients still relapse due to drug-resistant cancer cells.
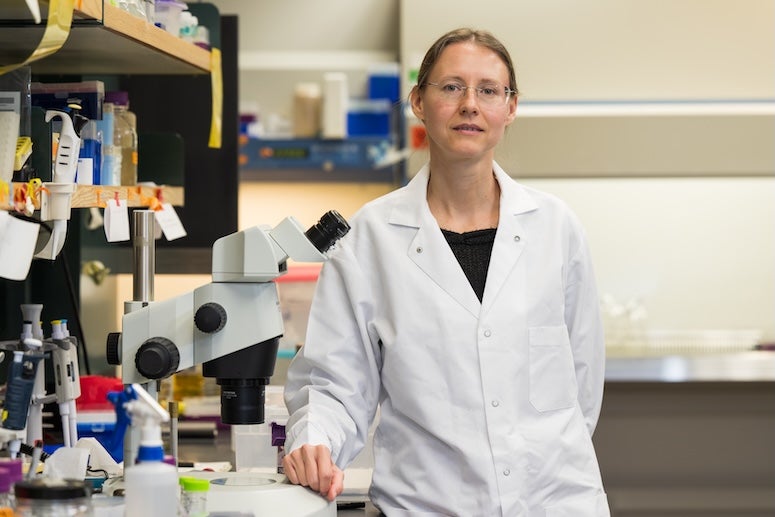
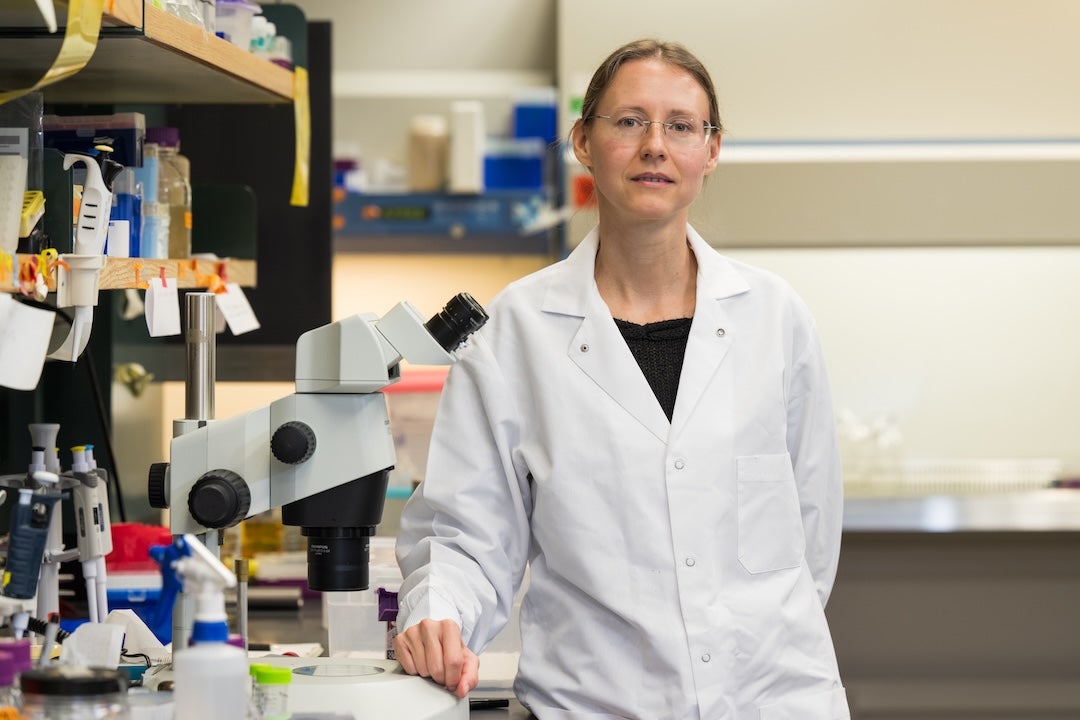
A research team led by Natasha Kirienko at Rice University is working to change that by turning the cancer cells’ own energy systems against them.
“Cancer cells grow so rapidly that they place a tremendous burden on their mitochondria — the cell’s energy producers — but they also disrupt the mechanisms that keep these mitochondria healthy,” said Kirienko, associate professor of biosciences and Cancer Prevention and Research Institute of Texas (CPRIT) Scholar. “We’ve discovered that targeting this mitochondrial dysfunction can selectively kill AML cells while leaving healthy blood cells unharmed.”
The work builds on Kirienko’s expertise in mitochondrial metabolism and cancer cell stress responses and is part of a collaborative effort that recently received a High Impact/High Risk grant from CPRIT. The project has the potential to fundamentally improve treatment outcomes for AML patients.
Kirienko’s collaborators include Natalia Baran, a leukemia specialist and assistant professor at University Hospital Bern in Switzerland, and Scott Gilbertson, the M.D. Anderson Professor of Chemistry at the University of Houston. Together, the trio brings complementary expertise to an ambitious plan: to optimize new mitochondria-targeting drugs, evaluate patient-specific responses and develop personalized drug combinations that minimize side effects and maximize survival.
“We want to get away from a one-size-fits-all model,” Baran said. “By testing how different mutations affect drug responses, we’re working toward therapies that are more tailored to individual patients, especially those whose cancer doesn’t respond to standard treatments.”
Another key part of the project involves preclinical testing using mice injected with human leukemia cells. These models allow researchers to better predict how new therapies will work in real patients.
“This kind of translational approach is essential,” Gilbertson said. “We’re not just testing molecules in a dish — we’re trying to understand how well they function in a living system and to optimize them for maximum therapeutic benefit.”
Ultimately, the team said they hope their work will lead to safer, more effective options for people with AML.
“This is about offering hope to patients who have exhausted standard treatments,” Kirienko said. “We’re not just looking to extend life but to improve its quality by reducing the toll of treatment itself.”
If successful, the team’s findings could yield a new class of cancer therapies with broader implications for other treatment-resistant cancers beyond leukemia. And for the thousands of Texans who will face a leukemia diagnosis this year, it represents a promising step forward.