Taking medications on time, in the right dose and for the prescribed duration can be challenging for patients, and failure to do so comes with steep costs, causing 10% of hospitalizations and billions in avoidable spending in the United States alone, according to some estimates. A team of Rice University scientists has developed a new drug delivery platform that could make it easier to complete a therapeutic regimen and even boost drug efficacy.

The research, published in Nature Nanotechnology, introduces a peptide hydrogel that functions as a three-dimensional net which controls the rate of release across a range of medication types, including small-molecule drugs and biologics like insulin and antibodies. The system, called self-assembling boronate ester release or SABER, uses reversible chemical bonds between two chemical groups — one located on the peptide and one on the drug molecule — to greatly extend the duration of drug release. Consequently, instead of passing quickly through the net, the drug gets temporarily “stuck” each time it binds to the peptide, slowing its passage out of the hydrogel.
In one set of experiments, the researchers formulated a tuberculosis-treating drug into a hydrogel and used it to treat infected mice. A single injection of the drug-laden hydrogel outperformed almost daily oral administration of the medication over a two-week period. In another set of experiments, insulin packaged in SABER hydrogels successfully controlled blood sugar levels in diabetic mice for six days. To put that in perspective, treating the animals with the maximum tolerated dose of insulin administered the conventional way would only guarantee blood sugar level control for four hours.
The SABER platform could improve treatment adherence and outcomes for existing therapies and open new possibilities for more precise delivery in areas like cancer immunotherapy, where controlling the timing and location of drug release could help reduce harmful side effects.

Brett Pogostin, a Rice doctoral alum who led the development of SABER, began working on self-assembling peptides as an undergraduate. At Rice, he was jointly advised by chemist Jeffrey Hartgerink and bioengineer Kevin McHugh, and his work sought to bridge foundational materials research and biomedical applications.
“I was interested in bridging the two labs and figuring out how I could combine my chemistry and bioengineering interests to do something impactful,” said Pogostin, who is the first author on the study.
The initial insight behind SABER was sparked by a drug delivery course taught by McHugh, when Pogostin learned about dynamic covalent bonds used in glucose sensing. These bonds reversibly form and break apart — a quality that inspired him to adapt the concept for drug delivery.
“A major challenge of using hydrogels in drug delivery is that they often rapidly release small drugs,” Pogostin said. “You can imagine you’re a fisherman out at sea and you’re trying to catch minnows but you’re using a net made for tuna. The minnows swim right through.”
Pogostin hypothesized that dynamic covalent chemistry could be used to make the hydrogel net “sticky.” By chemically modifying the hydrogel to interact with boronic acid-bearing drugs, he was able to slow release through reversible bonding.

“The rate of drug release would be dictated by the rate of that dynamic covalent bond breaking and reforming,” he said. “And it actually worked really well.”
The team demonstrated the platform in two different use cases. Tuberculosis remains one of the world’s deadliest infectious diseases — not for lack of effective treatments but because patients in low-resource settings often struggle with access, storage and adherence to long treatment schedules. SABER not only simplified dosing but enhanced the efficacy of the drug.
On the biologics side, the researchers turned to insulin, a notoriously difficult-to-dose hormone that requires careful timing. In scenarios where cold storage and frequent injections are barriers, the benefits to Type 1 diabetes patients of a simpler and longer-acting way to administer insulin could be significant.
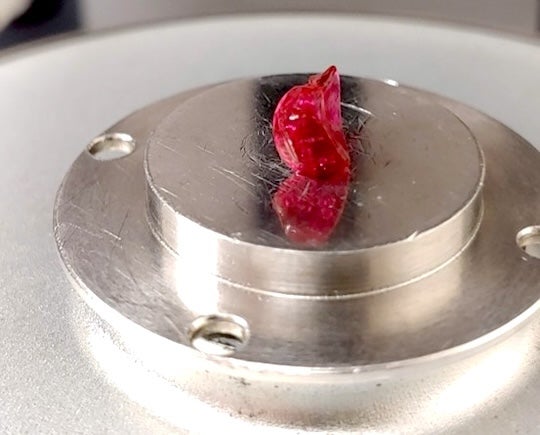
Because the hydrogel is made of amino acids, it breaks down naturally in the body. After injection, it forms a small, temporary nodule under the skin that gradually dissolves with no toxic byproducts.
The path from initial idea to developed platform was anything but straightforward, requiring broad interdisciplinary coordination. Pogostin consulted Rice chemist Zachary Ball on boronic acid interactions and worked with collaborators at Johns Hopkins University who helped identify tuberculosis as a priority use case.
Measuring drug concentrations in mouse blood required custom workflows and help from Rice’s Shared Equipment Authority. Early in the project, Pogostin spent months troubleshooting a synthesis problem only to discover the solution was heating the material to remove a stubborn protecting group.

“It was an unglamorous solution, but that little increase in temperature made the whole thing possible,” Pogostin said. “The solution to almost every challenge was to find someone who was an expert in what we wanted to do and bring them in.”
Collaboration thrived also due to the setting with many of the labs involved in the project being housed in Rice’s Bioscience Research Collaborative building, a space designed to facilitate the free exchange of ideas and expertise sharing among researchers.
“Answers arose naturally out of the people and the place,” Pogostin said.
“Brett really drove this project in a way that is, in my experience, unusual for a graduate student,” said Hartgerink, who is a corresponding author on the study. “It’s a very versatile approach. You can make both small-molecule drugs and very large biologics sticky with the type of chemistry that Brett developed.”
McHugh, who is also a corresponding author on the study, described the system’s tunability in terms of staging a “handshake” between chemical groups, or having “the right handle” to make possible a specific interaction.
“We can install a ‘handle’ on whatever drug we are interested in — assuming it does not undermine that molecule’s activity — to couple it to the delivery platform,” McHugh said, adding that his research group is especially interested in protein drug delivery, e.g. antibodies, hormones, enzymes and more.
The team’s research was supported by multiple collaborators and represents what McHugh described as “generation one” of the SABER system, with ongoing work underway to make it even more widely applicable. Both the Hartgerink and the McHugh labs are now refining the system and exploring next-generation applications.
Hartgerink, for example, is looking into how SABER could be applied in the context of cancer immunotherapy, where he sees the potential impact of the platform as “quite exciting.”
Pogostin, now a postdoctoral fellow at the Massachusetts Institute of Technology funded by a K00 award from the National Cancer Institute, continues to draw on his interdisciplinary mindset bridging chemistry and bioengineering as he applies himself to new areas of research, specifically immunology.
“What I’m really passionate about right now is cancer prevention — trying to think about how we can use materials to prime the immune system to prevent cancer from ever happening as opposed to just treating it,” Pogostin said.
The research was supported by the National Science Foundation (2203948), the National Institutes of Health (F99CA284262, R35GM143101, R01DE021798, R01DE030140, R61-AI-161809), the Cancer Prevention and Research Institute of Texas (RP190617, RR190056) and the Welch Foundation (C-1680). The content herein is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations and institutions.
- Peer-reviewed paper:
-
Nanofibrous supramolecular peptide hydrogels for controlled release of small molecule drugs and biologics | Nature Nanotechnology | DOI: 10.1038/s41565-025-01981-6
Authors: Brett Pogostin, Samuel Wu, Michael Swierczynski, Christopher Pennington, Si-Yang Li, Dilrasbonu Vohidova, Erin Seeley, Anushka Agrawal, Chaoyang Tang, Marina Yu, Arghadip Dey, Sofia Hernandez, Jacob Cabler, Omid Veiseh, Eric Nuermberger, Zachary Ball, Jeffrey Hartgerink and Kevin McHugh
https://www.nature.com/articles/s41565-025-01981-6 - Access associated media files:

