As measles cases rise across Texas and the nation, a team of researchers at Rice University and the Houston Health Department is leveraging wastewater surveillance to detect the virus in the community. This innovative approach is part of the Houston Wastewater Epidemiology system and offers public health officials a powerful early warning system to track outbreaks and mobilize targeted interventions. The Houston Wastewater Epidemiology core team consists of interdisciplinary experts, including Lauren Stadler, associate professor of civil and environmental engineering; Katherine Ensor, the Noah G. Harding Professor of Statistics; and Loren Hopkins, chief environmental scientist at the Houston Health Department and professor in the practice of statistics and environmental analysis at Rice.
Houston Wastewater Epidemiology has been at the forefront of its field since the onset of the COVID-19 pandemic, and its work has contributed to developing one of the most advanced monitoring systems in the country. Houston Wastewater Epidemiology is also a Centers for Disease Control and Prevention-designated National Wastewater Surveillance System Center of Excellence, supporting research and innovation in wastewater surveillance nationwide.
“With infectious diseases like COVID-19, flu and RSV, wastewater surveillance has proven to be an efficient, timely and resource-effective tool,” Stadler said. “Now with measles cases on the rise, we are using the same approach to detect the presence of this highly contagious virus in Houston’s wastewater before outbreaks occur.”
Proven early detection capabilities
Recent findings from Houston Wastewater Epidemiology’s collaboration with Texas Epidemic Public Health Institute confirm the effectiveness of wastewater surveillance for measles. In January 2025, Houston Wastewater Epidemiology retrospectively tested wastewater samples collected across the city and analyzed them for measles.

“Wastewater collected on Jan. 7 tested positive for measles, while the first confirmed case was not officially reported until Jan. 17,” Stadler said. “The cases were travel-related and did not lead to an outbreak, but our detection validates the power of wastewater surveillance as a potential early warning tool.”
With measles actively circulating in Texas, the Houston Wastewater Epidemiology team has expanded monitoring across the city. A third case of measles was recently reported in Houston in March — an unvaccinated infant who was exposed to measles during international travel. No wastewater detections have been reported that are associated with this case since the patient wore diapers and was unlikely to be directly contributing to the wastewater stream.
“We are in full preparedness mode,” Hopkins said. “If measles reaches Houston, wastewater surveillance will help direct resources to impacted communities and encourage vaccinations.”
The measles-mumps-rubella (MMR) vaccine has been in use for decades. One dose provides 93% protection while two doses offer 97% protection.
“This vaccine is incredibly safe and highly effective,” Hopkins said. “With such a contagious virus, it is critical that we get immunization rates back up to protect our communities.”
How wastewater surveillance detects measles
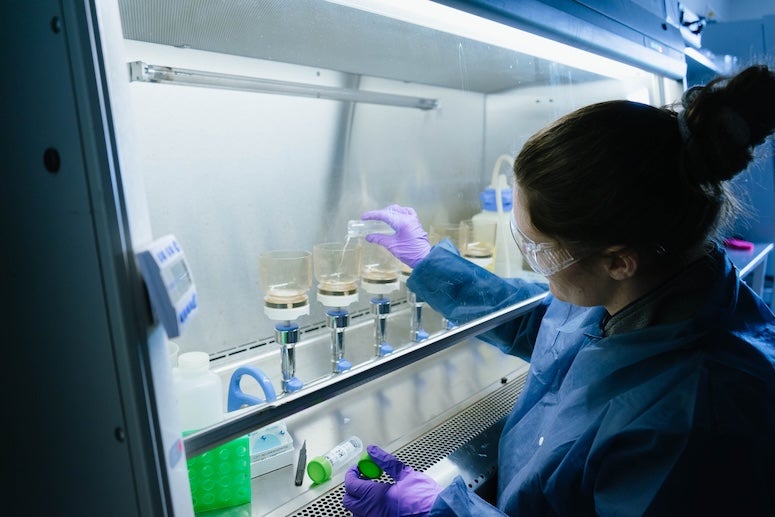
Stadler’s lab has developed highly sensitive assays to detect measles viruses in wastewater. The process begins with collecting wastewater samples from Houston’s 38 wastewater treatment plants as well as from targeted sites that serve especially vulnerable populations such as K-12 schools, nursing homes and homeless shelters. Once collected, the samples are concentrated to isolate the viral genetic material. Researchers then use droplet digital polymerase chain reaction technology to amplify the virus’s unique RNA signature, allowing for precise detection.
A key breakthrough in Stadler’s method is the ability to distinguish between wild-type measles, which signals infectious cases, and the vaccine strain, preventing false alarms from vaccine-related shedding. A recent paper published in Environmental Science & Technology outlines how a team led by Jingjing Wu, a postdoctoral scholar in Stadler’s lab, and members of Todd Treangen’s group in the computer science department at Rice, developed and validated an assay to differentiate these strains in wastewater with an eye toward enhancing surveillance of vaccine-preventable diseases. Stadler’s lab successfully validated the assay using wastewater from a Chicago facility during an active measles outbreak.
“When people get the measles vaccine, they shed an attenuated, noninfectious version of the virus,” Stadler said. “Our lab developed a method to differentiate between vaccine-derived shedding and actual measles infections, which is critical for accurate and timely public health responses.”
Why wastewater surveillance matters
Measles, which was declared eliminated in the U.S. in 2000, has resurged due to declining vaccination rates with misinformation largely driving this trend. National immunization levels have dipped below the 95% threshold required for herd immunity, putting children and vulnerable populations at increased risk. Texas has already reported numerous confirmed measles cases, including the deaths of two unvaccinated children.
“Measles is extremely contagious — even more contagious than COVID-19,” Stadler said. “With vaccination rates dropping, we have been preparing for an uptick in outbreaks. Wastewater surveillance allows us to track infections without requiring individuals to seek testing, making it an unbiased and privacy-protecting method for public health monitoring.”
Unlike clinical reporting, which depends on symptomatic individuals seeking medical attention, wastewater surveillance captures data from an entire community, detecting viruses shed through urine and feces. The method allows researchers to identify infections, in some instances before individuals show symptoms or visit health care providers, enabling early intervention.
The Houston Wastewater Epidemiology team is available for interviews about wastewater surveillance for infectious diseases. For inquiries or to schedule an interview, please contact Alex Becker at alex.becker@rice.edu or 713-348-6794.