By: Raji Natarajan
Special to Rice News
Impaired neuromusculoskeletal function due to conditions such as stroke, osteoarthritis, cerebral palsy, Parkinson’s disease, limb amputation, spinal cord injury, traumatic brain injury and cancer is a leading cause of disability and affects roughly 1.7 billion people worldwide, including 19% of the U.S. adult population. Researchers led by Rice University’s Benjamin J. Fregly have developed a treatment design software that implements a novel personalized medicine approach for addressing this important societal problem. Called the Neuromusculoskeletal Modeling (NMSM) Pipeline, the software allows researchers to work in collaboration with clinicians to construct personalized neuromusculoskeletal computer models of individual patients (i.e., digital twins) then use those models to design orthopedic surgery, physical therapy or neurorehabilitation treatments that maximize each patient’s functional outcome. This work was recently published in the Journal of NeuroEngineering and Rehabilitation.
Movement impairments produce not only physical challenges but also a decreased quality of life due to increased health care costs, lower work productivity, reduced independence and increased risk of chronic conditions such as heart disease and diabetes. Studies show that patients are often dissatisfied with orthopedic surgeries, physical therapy regimens or neurorehabilitation interventions designed using existing approaches when they do not achieve their desired level of functional improvement, especially for performing simple everyday activities.
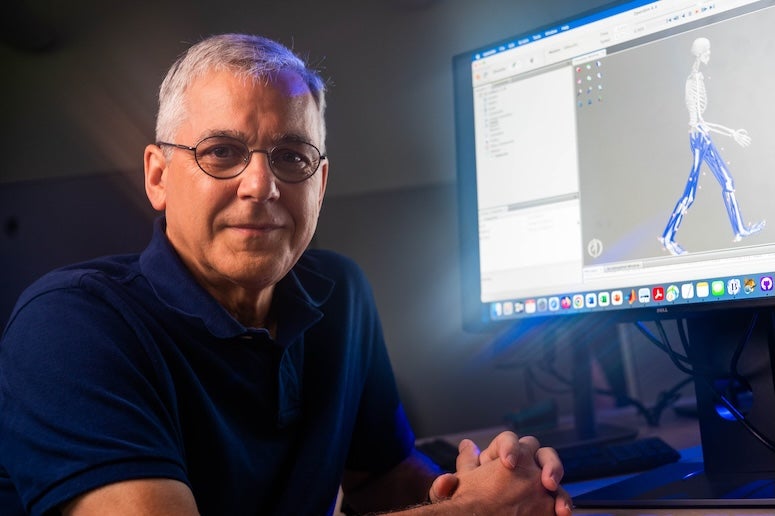
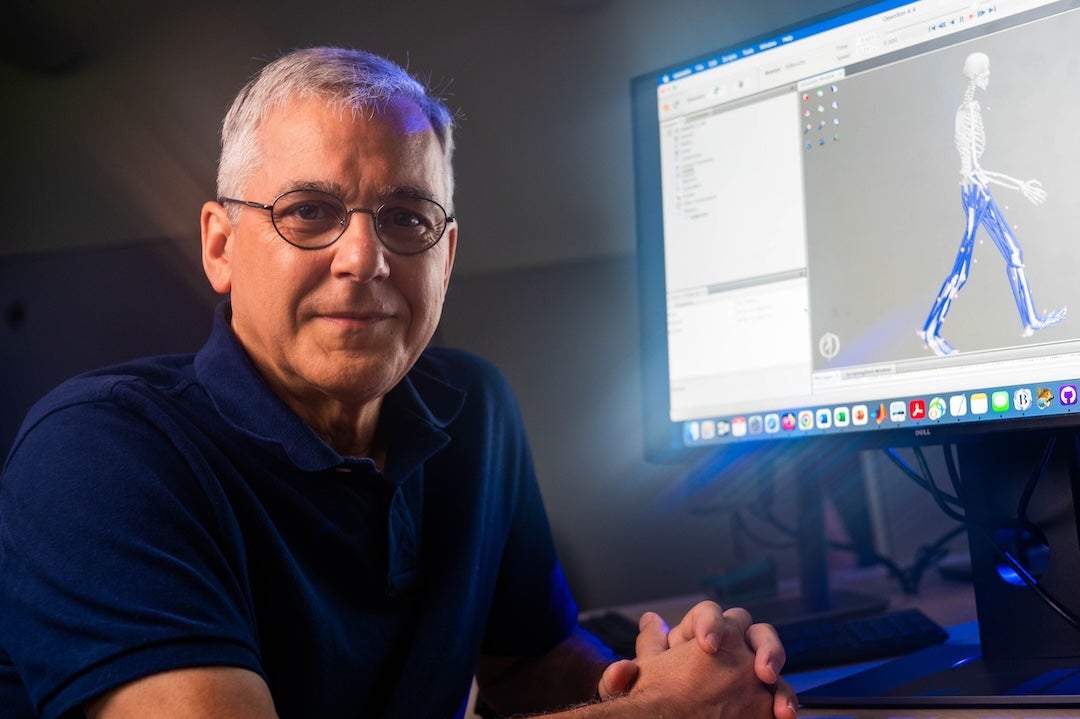
“A significant reason for suboptimal functional recovery is that existing treatment design methods do not adequately address the unique clinical situation and specific needs of each patient,” said Fregly, the Trustee Professor of Mechanical Engineering and Bioengineering and a Cancer Prevention and Research Institute of Texas Scholar in the George R. Brown School of Engineering and Computing at Rice. “Our goal was to create a cutting-edge physics- and physiology-based computational tool that would model each patient’s unique anatomy and physiology with sufficient accuracy to predict the patient’s post-treatment movement function with high reliability. The tool could then allow clinicians to plan, develop and test a wide range of potential treatments, ultimately identifying the one that was most likely to produce the best functional outcome for the patient.”
Combining physics, physiology and neuroscience to create a personalized modeling solution
The human neuromusculoskeletal system resembles a well-designed mechanical system, suggesting that it can be modeled using laws of physics coupled with principles of physiology and neuroscience, and that computational technologies that revolutionized the design of airplanes, automobiles and heavy equipment over the past 25 years can also revolutionize the design of surgical and rehabilitation treatments for movement impairments.

Fregly and his team at Rice leveraged this tried-and-tested engineering design optimization approach to build on the functionality and reliability of an existing open-source musculoskeletal modeling software package called OpenSim developed by researchers at Stanford University. Their new open-source, MATLAB-based software package called the NMSM Pipeline features two new state-of-the-art tool sets — a model personalization tool set for creating “digital twins” of patients and a treatment optimization tool set for performing virtual treatments on the patient’s digital twin.
The software is the first of its kind to allow researcher-clinician teams to personalize a broad array of anatomical, physiological and neurological properties to patient movement data, then use the personalized model to design actual clinical interventions. Unlike “black box” machine learning models, physics-based models require much less data to develop and can extrapolate accurately to predict novel situations (such as post-treatment) that are outside the training boundaries.
The model personalization tool set factors each patient’s unique anatomy, physiology and neural control properties to model their pretreatment movement data and numerical optimization to personalize an OpenSim musculoskeletal computer model, so it represents the patient’s joint structure, muscle-tendon, neural control and foot ground contact properties. By modeling these differences reliably, this tool set accounts for how a patient’s unique characteristics should affect the design of the patient’s clinical intervention.
The treatment optimization tool set combines a patient’s personalized neuromusculoskeletal computer model with a different type of numerical optimization to predict how a patient’s neural control and anatomy should be altered, or how an external device or implant should be designed or controlled to maximize the patient’s movement function after treatment. This promising tool set allows for fine-tuning the implementation of existing treatments or for identifying entirely new treatments that have not been identified previously.
A case in point is a personalized rehabilitation treatment for medial knee osteoarthritis designed by Fregly’s lab in 2007 and recently repredicted using the NMSM Pipeline. This walking modification corrected the patient’s knees by as much as an invasive orthopedic surgery. Notably, this new rehabilitation treatment had been “hiding in plain sight”— it took a predictive walking simulation performed using a personalized computer model to bring it to light.
The primary benefits of the NMSM Pipeline software are its extensive functionality, predictive capabilities, ease of use and computational speed. With processed movement data collected from a patient prior to treatment, a researcher-clinician team can create a personalized neuromusculoskeletal computer model of the patient in as little as one day, making the concept of a “digital twin” a reality. Though the subsequent treatment design process currently takes longer, development of best practices for simulating different types of clinical problems (e.g., stroke neurorehabilitation versus pelvic cancer surgery) could permit the entire computational treatment design process to be performed in a matter of days. Better yet, this two-step personalized computational treatment design process can be performed without writing a single line of computer code, making it accessible to individuals with only minimal engineering training.
“We are excited about the NMSM Pipeline’s potential to transform the treatment design landscape for movement impairments,” Fregly said. “We hope that by making high-end neuromusculoskeletal modeling, simulation and optimization capabilities easy to use, computationally fast and freely available, the medical and research communities will begin to explore how objective predictions of a patient’s post-treatment movement function based on personalized models can augment — and hopefully improve — subjective predictions based on clinical experience.”
This work was funded by grants from the National Institutes of Health, the Cancer Prevention and Research Institute of Texas and the National Science Foundation. The content herein is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations and institutions.