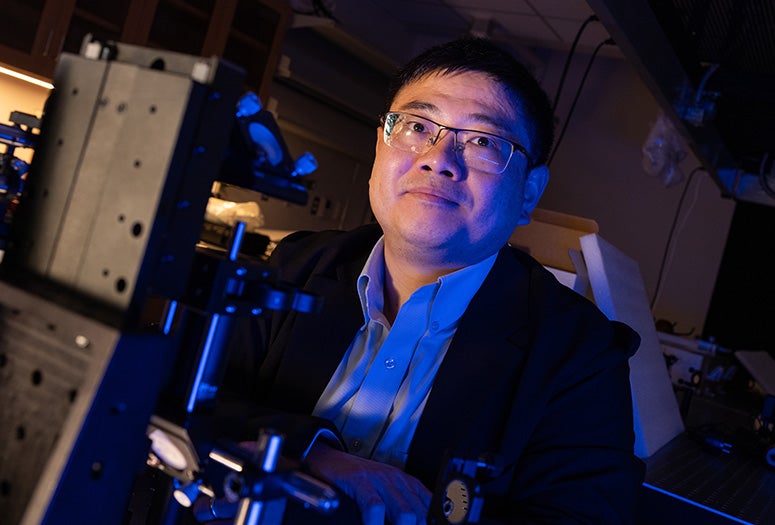
Lei Li, assistant professor of electrical and computer engineering at Rice University, has received a National Science Foundation CAREER Award to develop a new generation of wearable medical imaging technology capable of visualizing deep tissue function in real time.
The highly competitive five-year NSF grants are given to early career faculty members who demonstrate the potential to serve as academic models and leaders in research and education.
Li’s project centers on photoacoustic imaging, a technique that merges light and sound to produce high-resolution images of structures deep inside the body. In photoacoustic imaging, pulses of laser light are absorbed by tissue, leading to a rapid temperature rise. The heat causes the tissue to expand by a fraction — generating ultrasound waves that travel back to the surface, where they are detected and converted into an image.
This approach captures far more detail than conventional ultrasound and can visualize biological structures without the use of dyes or contrast agents. However, current photoacoustic systems rely on large arrays of sensors, making them bulky, expensive and impractical for everyday or at-home use.
Li’s research addresses this limitation by rethinking how the acoustic signals are captured and decoded. Instead of using hundreds of separate sensors, his team is developing a new method that allows just one sensor to capture the same information. The key is a specially designed encoder that tags each incoming sound wave with a unique spatiotemporal signature, along with a reconstruction algorithm that can later interpret and decode the signals.
“Reducing the number of detection channels from hundreds to one could shrink these devices from bench-top systems into compact, energy-efficient wearables,” Li said. “That opens the door to continuous health monitoring in daily life — not just in hospitals.”
The proposed system combines hardware and software innovation: A physical encoding medium that shapes the acoustic signals and mathematical tools that decode them into images. Together, these advances could lower the size, cost and power consumption of imaging systems by several orders of magnitude, paving the way for their use in telemedicine, remote diagnostics and real-time disease monitoring.
Rice offers a unique environment for this work, with close proximity to the Texas Medical Center and a strong ecosystem of medical imaging research and commercialization. Li’s lab also collaborates with clinicians to explore how the miniaturized technology could help monitor cancer treatment and other conditions over time.
“This is about giving people access to powerful diagnostic tools that were once confined to hospitals,” Li said. “If we can make imaging affordable, wearable and continuous, we can catch disease earlier and treat it more effectively.”