A new method developed by a research team led by Rice University’s Jerzy Szablowski offers hope for treating brain disorders through gene therapy. The innovative approach could transform treatments for inherited conditions and mental health issues by targeting specific regions of the brain with newfound precision. The researchers’ work was recently published in Nature Communications.
Gene therapy can potentially correct genetic defects, but delivering therapeutic genes to the brain has posed significant challenges. Traditional noninvasive methods lack efficiency, target the whole brain versus only the diseased regions and can affect healthy tissues, leading to potential toxicity.
“A commonly used alternative is to drill a hole in the skull and insert a needle into the brain, but that surgery is invasive and carries its own risks,” said Szablowski, an assistant professor of bioengineering.
The research team has developed a process that allows the vectors, or tools used to deliver genetic material into brain cells, to enter targeted regions while preventing cells from bleeding. The technique involves injecting modified gene delivery vectors into the bloodstream, enabling them to cross into the brain.
Some vectors used by clinics called adeno-associated viral vectors (AAVs) can enter the brain after focused ultrasound treatment, but they tend to enter the brain with limited efficiency and transduce many other tissues within the body. The researchers have modified the AAVs to allow them the opportunity to advance more efficiently.
The researchers hypothesized that by modifying the coat of the vector they could find protein sequences that result in improved delivery to the brain, but only in ultrasound-stimulated regions. Moreover, they theorized that they could locate vectors that can simultaneously reduce transduction of the liver, which is one of the main targets of common gene delivery vectors and one of the largest sources of toxicity in gene therapies.
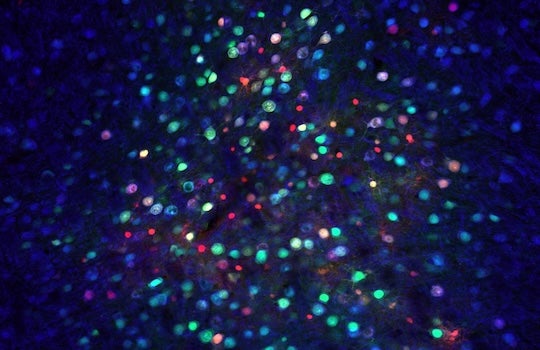
“To identify the best vectors, we injected 1.3 billion variants into mice," said Richard Li, the study’s lead author. The researchers then stimulated specific brain regions with ultrasound to enable delivery into the specific brain regions.
“By extracting the vectors that made it into the brain, we discovered thousands of promising candidates,” Li said.
Through rigorous testing, the researchers identified several vectors that demonstrated enhanced brain delivery and minimized liver targeting.
Engineering gene therapy vectors has been done for years, promising results with the potential to treat disorders affecting the whole brain, according to Szablowski. "This work is the first time engineered vectors and focused ultrasound delivery have been combined,” he said.
The novel method presents a noninvasive way to deliver genes to specific brain sites, making it particularly suitable for treating disorders that occur in specific brain areas such as psychiatric disorders. The team’s research showed that combining ultrasound with engineered vectors improved the specificity of brain versus liver delivery by around 1,000-fold compared to the clinically used AAVs without focused ultrasound treatment.
“This is an important improvement because higher liver transduction can limit toxicity,” Szablowski said. “And the improved efficiency of brain delivery means that lower doses of vectors are required, potentially reducing the cost of gene therapy.”
The research team includes Rice bioengineering graduate student Manwal Harb; former Rice research assistant James S. Trippett; Ph.D. candidates in biology at the California Institute of Technology Hongyi R. Li and John E. Heath; and Mikhail G. Shapiro, professor of chemical and medical engineering at Caltech.

