Synthetic biologists at Rice University are embarking on a three-year project to create “genetically encoded antibiotics,” strands of RNA that bacteria will readily copy and share that will selectively kill only disease-causing, pathogenic bacteria.
“Most bacteria pose no danger to human health,” said James Chappell, an assistant professor of biosciences and bioengineering at Rice. “The question for us as synthetic biologists is, ‘Can we create genetic programs that move through microbial communities and precisely remove only the bad actors from those communities?’”
Thanks to a $1.5 million grant from the Kleberg Foundation, Chappell’s lab and the lab of Rice bioscientist and bioengineer Jonathan “Joff” Silberg are getting a chance to test their idea of combating antibiotic resistance by enlisting the aid of bacteria that either benefit humans or pose no threat to them.
In prototype tests, they showed they could design RNA programs that were highly targeted and potent, killing 99.99% of “bad actor” pathogens within a matter of hours. In the three-year project, they also plan to partner with Dr. Pablo Okhuysen from the University of Texas MD Anderson Cancer Center to design RNA antibiotics that are effective against diarrhea-causing E. coli, as well as RNA drugs that selectively kill the opportunistic Lactobacillus iners, a pathogen that has been associated with cervical cancer radiation therapy resistance.
Another project aim is to establish “design rules” for RNA antibiotics, determine their potency and build an automated platform capable of designing inexpensive, tailored RNA antibiotics for individual patients within a matter of days.
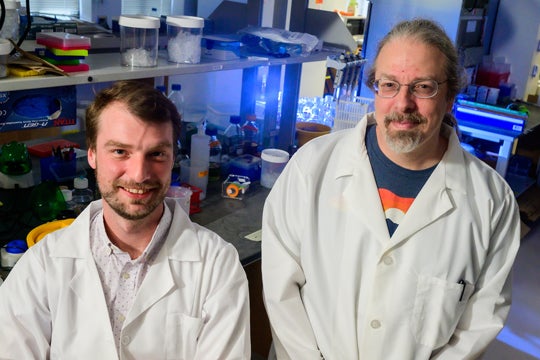
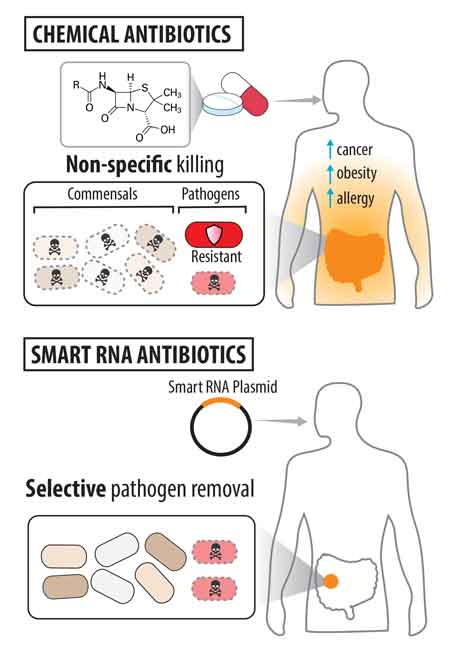
“Traditional antibiotics are great,” Chappell said. “They kill bad actors. But they are usually systemic. So they wipe out all of the good bacteria as well as the bad bacteria. We’re trying to be much more specific.”
Silberg said the idea came out of conversations during almost daily walks around the Rice campus during the pandemic.
“We were all de-densifying, and we became walking buddies,” Silberg said. “We ended up walking loops. It felt like a bunch of days each week. And this was the pandemic project that came out of that.”
Chappell’s lab specializes in creating genetic programs using molecules of nucleic acid called RNA. Like DNA, RNA is present in all living cells. RNA is structurally similar to DNA, life’s medium of choice for permanently storing information. RNA is the medium used by cellular machinery that “reads” DNA and “writes” actionable instructions for other parts of the cell.
“For a long time, people just thought of RNA as this passive intermediate going from DNA to proteins,” Chappell said. “But we now know it actually does a lot more things. It can sense things, regulate gene expression and catalyze reactions. It’s a very functionally versatile molecule.”
One focus of Silberg’s lab has been on using synthetic biology to probe microbial communities and better understand how they work collectively in nature to drive processes that far exceed their scale. Soil bacteria, for example, play critical roles in soil development, water quality, crop yields and greenhouse gas production. His group has created bioelectronic sensors, cells that can measure processes, record and store data about what they sense and even communicate that information in real-time.
The idea that arose during their pandemic walks was to create RNA programs that can kill bacteria like traditional antibiotics but in a targeted way that is fundamentally different from traditional antibiotics.
“The traditional way is to discover a chemical that kills bacteria en masse and give that as a drug,” Chappell said.
Prior to the widespread use of antibiotics after World War II, up to 25% of deaths were attributed to infections. The non-specific nature of antibiotics and their overuse has led to an explosion of drug-resistant pathogens. And with antibiotic discovery rates diminishing and the cost of drug development skyrocketing, public health officials have begun warning of a rapidly approaching “post-antibiotic” era.
Silberg said genetically encoded antibiotics would limit the emergence of drug resistance by only affecting targeted pathogens.
“Antibiotic stewardship is a real problem,” Silberg said. “We throw chemical antibiotics at animals and at humans. They're everywhere, and they're affecting microbes wherever they are. The synthetic biology approach is different because it allows you to create something that's actually not bad for microbes until it bumps into bad microbes.”
To deliver that targeted approach, the lethal programming is designed to go into action only when it sees “bad actor” genes that are found only in pathogenic microbes.
Silberg said the RNA instructions can effectively be, “That thing that’s different about bad E. coli … turn on the antibiotic when you see that.”
Chappell said, “It's kind of turning the instructions in the bad cells against themselves. We use a unique signature, something that’s essential for that pathogenic lifestyle, and we boot the program off of that.”
- Image downloads
-
https://news-network.rice.edu/news/files/2023/03/0307_ANTIBIOTIC-jcjsFit11-lg-1.jpg
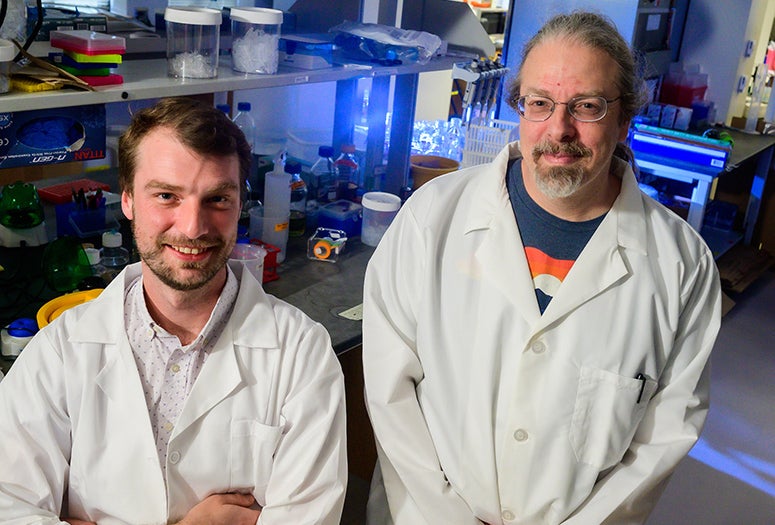
CAPTION: Rice University bioscientists James Chappell (left) and Joff Silberg aim to create “genetically encoded antibiotics,” strands of RNA that bacteria will readily copy and share. The RNA will selectively kill disease-causing bacteria thanks to a triggering mechanism that will be activated by “virulence genes” or other biomarkers found only in bacterial pathogens. (Photo by Jeff Fitlow/Rice University)
https://news-network.rice.edu/news/files/2023/03/0307_ANTIBIOTIC-f1v-lg.jpg
CAPTION: An illustration of the differences between traditional antibiotic drugs (top) and “smart,” genetically encoded antibiotics that are designed to selectively kill only disease-causing bacterial pathogens. (Figure courtesy of Chappell Lab/Rice University)
https://news-network.rice.edu/news/files/2023/03/0307_ANTIBIOTIC-f1h-lg.jpg
CAPTION: An illustration of the differences between traditional antibiotic drugs (left) and “smart,” genetically encoded antibiotics that are designed to selectively kill only disease-causing bacterial pathogens. (Figure courtesy of Chappell Lab/Rice University) - Related stories
-
Rice team eyes cells for sophisticated data storage – Aug. 18, 2022
https://news.rice.edu/news/2022/rice-team-eyes-cells-sophisticated-data-storageRice bioscientist Chappell awarded Sloan Research Fellowship – Feb. 15, 2018
https://news2.rice.edu/2018/02/15/rice-bioscientist-chappell-awarded-sloan-research-fellowship/ - Links
-
Silberg Lab: https://www.silberglab.org
Chappell Lab: https://www.chappell-lab.org
Rice Department of BioSciences:https://biosciences.rice.edu
Wiess School of Natural Sciences: https://naturalsciences.rice.edu/
George R. Brown School of Engineering: https://engineering.rice.edu/
- About Rice
-
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation’s top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 4,240 undergraduates and 3,972 graduate students, Rice’s undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for lots of race/class interaction and No. 1 for quality of life by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger’s Personal Finance.