Team wins prestigious federal grant to pursue leadless, wirelessly powered system
A trio of faculty members at Rice University’s Brown School of Engineering will be part of a push by the Texas Heart Institute (THI) to further the development of their novel leadless, wirelessly powered pacemaker system.
The National Institutes of Health has awarded a prestigious four-year R01 grant for $2.4 million to Dr. Mehdi Razavi, a cardiologist, director of Electrophysiology Clinical Research and Innovations at THI and a frequent collaborator with Rice faculty and students. The grant will be administered by the National Heart, Lung and Blood Institute.
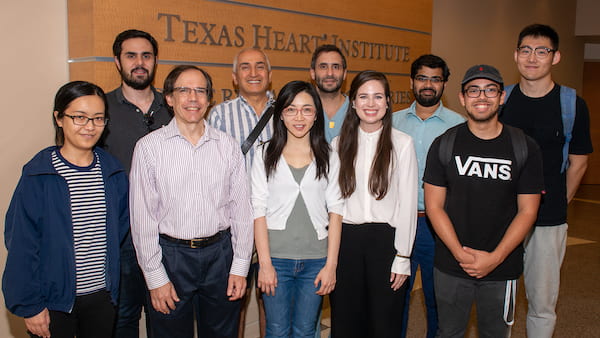
Members of the team that will continue to develop leadless, wirelessly powered pacemakers gathered at Texas Heart Institute. From left, front: Rice graduate student Yang Zhao, Joseph Cavallaro, Yingyan Lin, THI research engineer Allison Post, Rice graduate student Anton Banta; and back, Rice graduate student Romain Cosentino, Behnaam Aazhang, Dr. Mehdi Razavi, THI research engineer Mathews John and Rice graduate student Yue Wang. Courtesy of the Texas Heart Institute
The new pacemakers would allow simultaneous pacing and sensing from multiple sites in the heart to help reduce complications associated with traditional pacemakers. The pacemaker project was introduced at a 2017 conference and profiled by Rice News.
“Current wireless pacemakers can be effective for patients with certain types of atrial fibrillation and in patients with a medical condition or anatomy that blocks access to the vessels where traditional pacemaker leads are attached,” Razavi said. “However, if the patient needs dual-chamber pacing, we are forced to use a traditional pacemaker with leads.”
Pacemaker wires, known as leads, are prone to fracturing, dislodging and migrating away from their original locations, he said. “Our technology could overcome this problem and make wireless, leadless, battery-less pacemakers available to these patients,” Razavi said.

Mehdi Razavi

Behnaam Aazhang
Joseph Cavallaro, a Rice professor of electrical and computer engineering and of computer science and director of the Center for Multimedia Communication, and Yingyan Lin, an assistant professor of electrical and computer engineering,will contribute to the hardware development, along with Aydin Babakhani, a former Rice associate professor now at UCLA.
Behnaam Aazhang, Rice’s J.S. Abercrombie Professor of Electrical and Computer Engineering, is the university’s principal investigator and will lead the development of the data-driven algorithm, while Razavi will oversee device development and all preclinical studies.
“The key technologies include learning the status of the heart’s conduction pathway and intervening to correct any irregularities,” Aazhang said. “Real-time, closed-loop learning and control are critical steps. Low-power and micro-scale implementation of these control algorithms are the natural next steps.”
“This is a really exciting project as it brings together Rice expertise in many areas to collaborate on an important health care problem with THI and UCLA,” Cavallaro said. “I look forward to contributing to the embedded processor architecture and networking aspects of the project along with Yingyan and Behnaam on the sensing and machine learning and control.”

Joseph Cavallaro

Yingyan Lin
Pacemakers are used to treat heart rhythm problems, in which the heart beats too fast, too slow or irregularly, conditions collectively known as arrhythmias. They are commonly used to treat a slow heartbeat caused by an overdose of medicine, a heart attack or heart surgery.
An American physiologist built the first device referred to as an “artificial pacemaker” in 1932. Powered by a spring-wound, hand-cranked motor, the device was dismissed as nothing more than a gadget and met with opposition at a time when using technology to alter the natural course of life was highly controversial.
Pacemaker advances exploded in the late ’50s and early ’60s with several firsts, including pacemakers that were battery-operated and wearable, totally implantable and self-contained. New battery technology in the 1970s dramatically improved the lifespan of the pacemaker.
According to THI, current leadless systems can provide pacing to one chamber of the heart, but pacing therapy is typically delivered synchronously to multiple chambers. The bulky size and shape of new leadless pacemakers do not allow for multi-chamber pacing. Miniature, battery-less devices are being tested in clinical trials, but these devices can only deliver effective therapy in combination with another pacemaker.
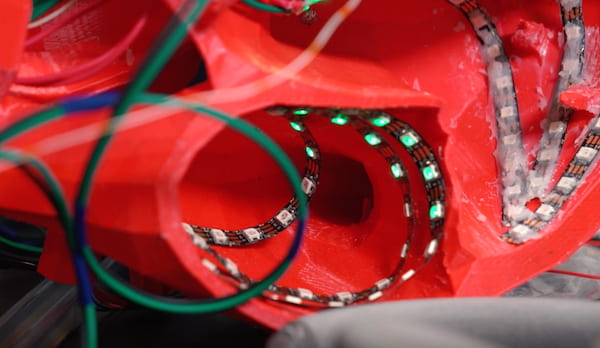
Rice engineering students demonstrated a next-generation, wireless pacemaker array at the 2018 George R. Brown Engineering Design Showcase. Their work helped lead to a federal grant to further develop leadless, wirelessly powered pacemakers. Photo by Brandon Martin
Razavi and his colleagues expect to overcome all of these challenges. The pacemaker will also learn from the data it generates, identify patterns and make adjustments to enable constant, optimal patient-specific therapy, according to THI research engineers.
“Our pacemaker is a diagnostic and treatment-delivering device with the ability to constantly read the heart’s electrical needs and self-correct or continuously adjust and recalibrate to deliver a unique pacing treatment, in real time, for each individual,” Razavi said.
Last year, the team received a $1.2 million National Science Foundation grant to advance machine learning systems relevant to the pacemaker network.
Razavi’s work with Rice faculty includes a recent collaboration with chemical and biomolecular engineer Matteo Pasquali on using carbon nanotube fibers to restore electrical conductivity to scarred heart tissue.
Earlier projects with students at the Oshman Engineering Design Kitchen include a needle platform for automated external defibrillators, shoes with sensors to help people with impaired sensation in their feet and a device to help obese patients breathe during surgery. Last year, he worked with Rice students to demonstrate the wireless pacemaker concept, a project that won the Excellence in Capstone Engineering Design Award at the annual George R. Brown Engineering Design Showcase.

