Rice’s decade-old anti-radiation work prompts possible strategy at MD Anderson Cancer Center
A Rice University chemist’s research conducted years ago to protect people from radiation poisoning due to nuclear fallout may now offer a glimmer of hope to patients with pancreatic cancer.

James Tour
Researchers at the University of Texas MD Anderson Cancer Center and Rice University have published a study on the novel use of amifostine, an approved intravenous drug used to protect healthy tissue in patients undergoing radiation therapy.
The results of new research led by MD Anderson radiation oncologist Dr. Cullen Taniguchi appear in an open-access paper in Nature’s Scientific Reports and are detailed in a report on MD Anderson’s Cancer Frontline blog.
Until now, if doctors used levels of radiation sufficient to destroy most tumors in the head of the pancreas, the radiation would also destroy the duodenum, which is the first stage of the small intestines.
But data from decade-old research by Rice University chemist James Tour suggested there might be another way. Tour, working at the time on a federal Defense Advanced Research Projects Agency grant, was looking for a nanoparticle-enabled method to curtail radiation poisoning in people exposed to nuclear fallout. Tests on an animal control group given amifostine orally proved far more interesting.
“Amifostine was developed at Walter Reed Medical Center in the 1970s and was identified as a radio protectant,” Tour said. “It is used intravenously to this day to protect patients.”
Working with Kathryn Mason, a now-retired faculty member at MD Anderson, Tour and his Rice group were testing antioxidant nanoparticles known as PEG-HCCs for their ability to quench the effects of radiation.

Dr. Cullen Taniguchi
“They helped a little bit, but nothing like the control,” he said.
Federal funding stopped at the end of the George W. Bush administration in 2008, he said.
“We had all this data, but not enough money to translate it,” Tour said. “And that was it,”
But Mason remembered. A few years later, she recommended that Taniguchi, a new recruit to MD Anderson, view the old data and visit Tour. Taniguchi, a radiation oncologist at MD Anderson and leader of the new study, immediately saw the potential for treating pancreatic cancer.
“Intravenous amifostine can cause severe nausea and hypotension, greatly limiting its use for patients,” Taniguchi said. “An effective oral version with less harmful side effects would allow us to extend this protection to more patients.”
“When you get a tumor in the head of the pancreas, you can’t do surgery, because the pancreas wraps around a huge artery,” Tour said. “You can’t do radiation because if you blast the tumor with the levels you’d need to kill it, you’d destroy the duodenum that connects the stomach to the small intestine.”
The duodenum contains groups of stem cells in a structure called a crypt. The crypts produce epithelial cells to replace those worn away by food that passes through the intestine.
“These crypts are the first thing to go when they’re exposed to radiation,” Tour said. “When they’re gone, bacteria on the food causes gastrointestinal syndrome.”
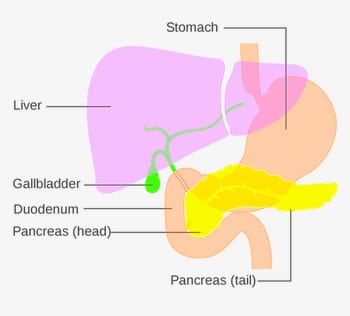 As it happens, amifostine taken orally is broken down by the enzymes in the duodenum. When the drug passes through the duodenum and jejunum, the alkaline environment there translates it into another drug, radio-protective WR-1065, precisely where it’s needed most. Ideally, a patient who takes amifostine a short time before radiation could better withstand a high-enough dose needed to eradicate the tumor, Tour said.
As it happens, amifostine taken orally is broken down by the enzymes in the duodenum. When the drug passes through the duodenum and jejunum, the alkaline environment there translates it into another drug, radio-protective WR-1065, precisely where it’s needed most. Ideally, a patient who takes amifostine a short time before radiation could better withstand a high-enough dose needed to eradicate the tumor, Tour said.
Even though amifostine is approved by the Food and Drug Administration, Tour warned that using it as part of a new strategy to treat pancreatic cancer is likely years away.
“This is not yet an approved treatment,” Tour said. “That won’t come until after the clinical trials are done.”
Jessica Molkentine, Tara Fujimoto, Thomas Horvath, Aaron Grossberg, Carolina Garcia Garcia, Amit Deorukhkar, Marimar de la Cruz Bonilla, Daniel Lin, Wai Kin Chan, Philip Lorenzi, Helen Piwnica-Worms and Robert Dantzer, all of MD Anderson, and Errol L.G. Samuel of Rice are co-authors of the paper.
The research was supported by the Cancer Prevention and Research Institute of Texas, the V Foundation, the Kimmel Foundation, the Sabin Family Foundation Fellowship, the McNair Foundation and the National Cancer Institute of the National Institutes of Health.

