Regenerative research will benefit cancer patients who suffer from dry mouth
Biologists, surgical oncologists and regenerative medicine specialists from Rice University, the University of Delaware and the Christiana Care Health System in Wilmington, Del., have begun a four-year program aimed at using cells to grow whole salivary glands that can replace those destroyed by cancer radiation therapy.
The research, which is funded by a $2.5 million grant from the National Institutes of Health’s National Institute of Dental and Craniofacial Research, could benefit thousands of cancer patients who suffer from xerostomia, or dry mouth.
Dry mouth is an especially severe problem for patients with cancers of the head and neck because the mouth’s saliva-producing acinar cells are particularly susceptible to radiation. As a result, about 40,000 head and neck cancer patients who undergo standard radiation therapy each year report serious problems with dry mouth. The condition can make it painful for patients to swallow, eat and even speak. It also causes accelerated tooth decay and oral infections.

Surgical oncologists and engineers from Delaware meet weekly by videoconference with Rice University researchers Daniel Harrington and Cindy Farach-Carson to discuss their efforts to grow whole salivary glands to replace those destroyed by cancer radiation therapy.
“We’ve already shown that we can harvest acinar cells prior to radiation therapy, grow them in the lab, implant them into test animals and maintain their ability to produce salivary enzymes,” said Cindy Farach-Carson, Rice’s Ralph and Dorothy Looney Professor of Biochemistry and Cell Biology and the principal investigator on the new grant. “In the next phase of the research, we want to show that we can make whole salivary glands that can integrate into the host and increase saliva production. To do that, we need more than just saliva-producing cells. We need nerves and ducts and blood vessels and all the other things that make up the gland itself.”
If the research is successful, it could pave the way for future clinical trials.
Farach-Carson, a biologist and longtime cancer researcher, said the regenerative salivary gland project is possible only because the research team includes experts in cell biology, clinical oncology and tissue engineering. For example, Rice’s project team includes co-investigator Daniel Harrington, faculty fellow in biochemistry and cell biology, who has expertise in polymer science and materials engineering.
Farach-Carson, who also serves as Rice’s vice provost for translational bioscience and as scientific director of Rice’s BioScience Research Collaborative, spends a good deal of her time extolling the benefits of research that crosses disciplinary and institutional boundaries. She said the salivary gland project is a perfect example of what can happen when experts from disparate fields come together to solve a common problem.
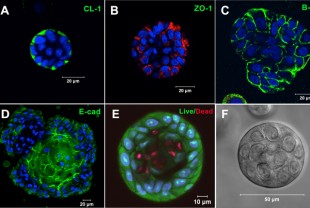
Researchers have shown that salivary cells cultured outside the body can be coaxed into forming organized structures similar to those found in the body. These images show cells marked with fluorescent dyes that identify specific proteins found in salivary tissues.
“This all began in 2005 when I went on sabbatical and was randomly assigned to share an office with Robert Witt, one of Delaware’s leading head and neck surgical oncologists,” Farach-Carson said. “My prior work had been with prostate cancer, so Bob and I traded stories about our previous work and found some common ground. Around that time, we also met Xinqiao Jia, a materials scientist at the University of Delaware who specializes in creating biomaterials for regenerative medicine.”
Witt, who directs the Head and Neck Multidisciplinary Center at Christiana Care’s Helen F. Graham Cancer Center, said, “There is currently no way to prevent or cure xerostomia for cancer patients who are undergoing radiation therapy. This is clearly a problem where regenerative medicine holds great promise for improving the quality of life for many people.”
In addition, the research could also benefit those with Sjögren’s syndrome, a chronic disease in which a person’s immune system attacks the body’s moisture-producing glands. Up to 4 million Americans live with Sjögren’s syndrome.
Jia, associate professor of materials science and engineering, said recreating the structure and function of whole salivary glands is a challenge.
“Every tissue in the body has unique requirements from its surroundings,” she said. “The biocompatible polymers we create at the University of Delaware can be tuned to match the structure of soft tissues in salivary glands. We can also incorporate specific biological cues to direct the growth and organization of the cells that are seeded into the polymers.”
Jia said her group works closely with their biological and clinical partners to identify the key properties that must be incorporated into the hydrogel polymers to direct cell organization and growth.
“This partnership over the past seven years has been incredibly rewarding for all of us,” Farach-Carson said. “Generous support from a patient of Dr. Witt provided the initial resources that enabled our early studies and brought us to where we are now. Without that help, we might never have reached this major milestone today.”


Leave a Reply